Fact Sheet: Miscarriage Management with Mifepristone
A recent article in Stateline described the troubles of Lulu, a woman suffering from a pregnancy loss who “couldn’t access the drug mifepristone — her preferred method of care — to help her body pass the miscarriage,” which Lulu states caused her to bleed for six weeks. The pro-abortion journalist then proceeded to blame state laws protecting unborn life and the politicization of abortion drugs for Lulu’s difficult experience.[1]
Unfortunately, there are many pro-abortion media sources and medical organizations spreading such misinformation who are more concerned with promoting abortion than safeguarding women’s health. They have also propagated the erroneous assumption that state laws protecting unborn life will limit miscarriage management. A straightforward reading of every state law restricting abortion of a living fetus, however, provides clear evidence that treatment of miscarriage is not prohibited by law (as the intent is to remove a deceased fetus).[2] Nonetheless, widespread confusion and anecdotes of denied care necessitate discussion of miscarriage treatment.
The terminology can be confusing, so it is important to be aware that “spontaneous abortion” describes a miscarriage, a pregnancy where the embryo or fetus has died naturally. “Induced abortion,” on the other hand, indicates that the pregnancy was intentionally ended through an external action (induced abortion sometimes being referred to simply as “abortion”). In other words, induced abortion occurs when the intent of the intervention is to produce the death of the unborn child. Procedures to manage a miscarriage are often the same as methods for inducing abortion, although the moral implications differ dramatically.
There are several standard options for miscarriage management. The American College of Obstetricians and Gynecologists (ACOG), a prominent professional organization, has provided comprehensive guidance for management of many obstetric and gynecologic conditions, including pregnancy loss.[3] “Accepted treatment options for early pregnancy loss include expectant management, medical treatment, or surgical evacuation,” ACOG explains.[4] They also recommend that patients “be counseled about the risks and benefits of each option.” Expectant management, watchful waiting in anticipation of a natural miscarriage without intervention, should “generally … be limited to gestations within the first trimester” according to ACOG. This is due to “a lack of safety studies of expectant management in the second trimester and concerns about hemorrhage.”[5] Surgical uterine evacuation, on the other hand, is recommended for “[w]omen who present with hemorrhage, hemodynamic instability, or signs of infection.”[6] Finally, ACOG’s advice for medication-managed miscarriage is as follows:
In patients for whom medical management of early pregnancy loss is indicated, initial treatment using 800 micrograms of vaginal misoprostol is recommended, with a repeat dose as needed. The addition of a dose of mifepristone (200 mg orally) 24 hours before misoprostol administration may significantly improve treatment efficacy and should be considered when mifepristone is available.[7]
As a board-certified OB-GYN practicing for over 30 years, when I have confirmed that a patient’s unborn child has died, I offer her several options. As mentioned previously, expectant management is one such option. Prior to our modern-day options for medical intervention, women’s bodies usually expelled miscarried tissue spontaneously and successfully. Women will often opt for this natural approach. If a woman does not want to wait, however, medication may hasten the process. Because I practice Hippocratic medicine and do not perform elective abortions, I have not registered to have access to mifepristone (see discussion below).
Misoprostol, on the other hand, is readily available, and I prescribe that medication for women who desire a medical intervention. Other women may prefer a minor surgical procedure — suction aspiration — which can be performed in an ambulatory surgical facility or in-office for physicians who have appropriate equipment and certification. If a woman chooses a non-surgical option, I remain available for any concerns. In such a case, I schedule a short-term follow-up to verify that the pregnancy tissue has been completely expelled and to confirm that my patient wants to continue with the intervention if tissue remains. If expectant management or medical treatment takes longer than desired or doesn’t work completely, the patient has the option of choosing a surgical procedure at that time.
Lulu’s complaint that she was required to bleed for six weeks after misoprostol does not reflect well on her OB-GYN. She could have opted for surgical completion of her miscarriage at any time. As ACOG recommends in their practice bulletin, I also do not recommend expectant management, or medications, for a patient who experiences a late pregnancy loss or encounters heavy bleeding. Such a patient is better served by surgical management to hasten resolution and minimize blood loss.
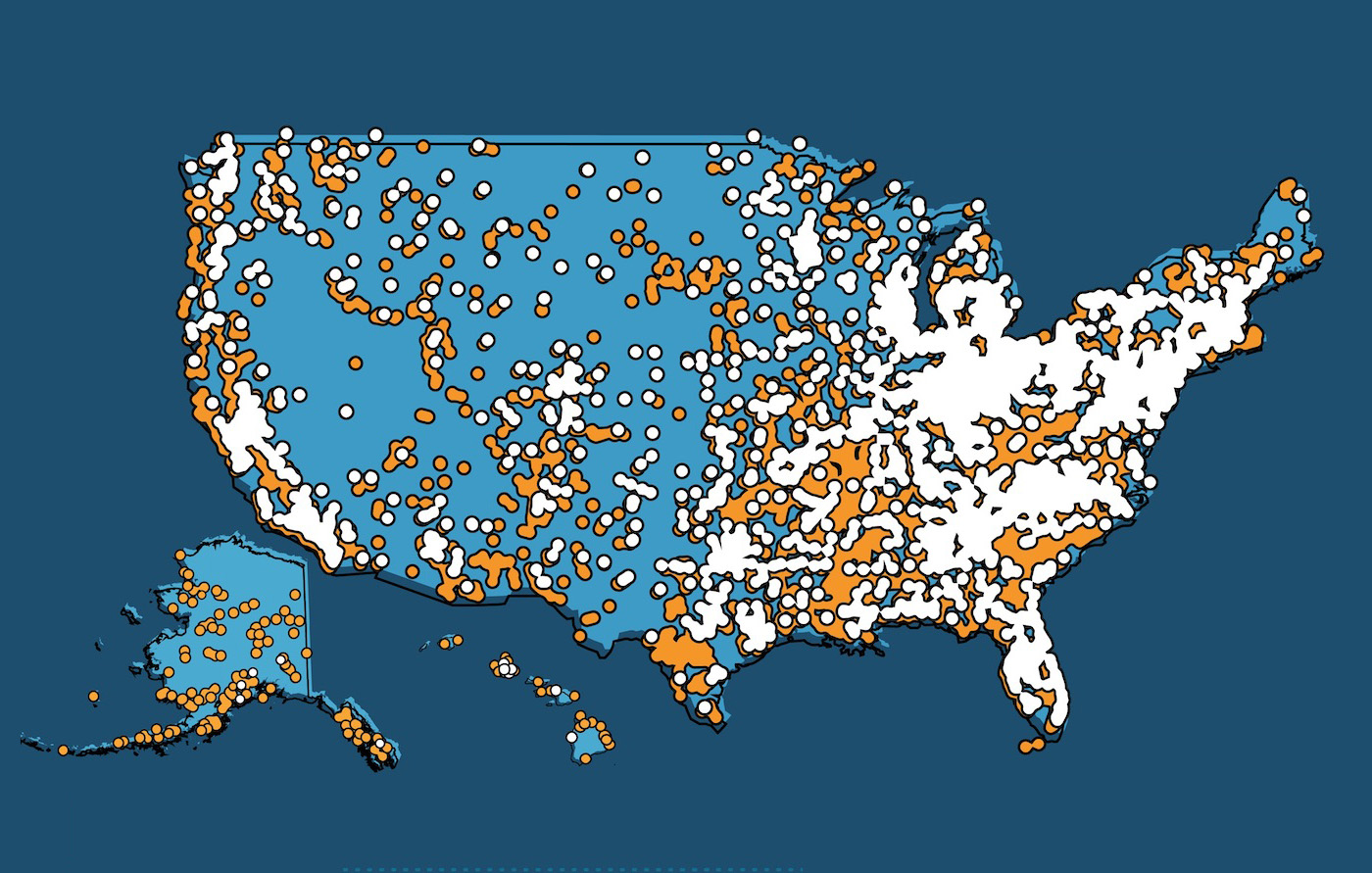
The FDA’s Risk Evaluation and Mitigation Strategy (REMS) requires a provider to be registered to prescribe and have access to mifepristone,[8] so the drug remains unavailable to most OB-GYNS. Only 7-14% of OB-GYNS surveyed indicate they would perform an elective abortion if requested by their patient, so most have not become registered providers of mifepristone.[9] There is limited data indicating that the addition of mifepristone may improve the efficacy of misoprostol in completing tissue evacuation during a miscarriage. A randomized-controlled trial comparing the two options for medical management found that 24% of women receiving misoprostol alone required surgical completion of their miscarriages, compared to 17% of the women receiving mifepristone plus misoprostol.[10] A comprehensive meta-analysis, however, documented that surgical treatment was the most effective of all the available options.[11]
Thus, if mifepristone is unavailable to an OB-GYN, his or her patients will not suffer, for there are several other effective options available for treating a miscarriage. Fearmongering about an inability to treat miscarriages in the aftermath of the Dobbs v. Jackson Women’s Health decision, which allowed legislative limits on electively ending unborn life, but posed no limitations on treating miscarriages, should be recognized for the ideologically driven, pro-abortion rhetoric that it is. The abortion drug mifepristone is not necessary for OB-GYNs to provide quality care to women suffering from heartbreaking pregnancy loss.
[1] Caitlin Dewey, “State, federal abortion rules prevent many women from accessing crucial miscarriage drug,” Stateline, October 20, 2023, https://stateline.org/2023/10/20/many-women-cant-access-miscarriage-drug-because-its-also-used-for-abortions/.
[2] Mary Harned and Ingrid Skop, “Pro-Life Laws Protect Mom and Baby: Pregnant Women’s Lives are Protected in All States,” Charlotte Lozier Institute, September 11, 2023, https://lozierinstitute.org/pro-life-laws-protect-mom-and-baby-pregnant-womens-lives-are-protected-in-all-states/.
[3] ACOG Committee on Practice Bulletins—Gynecology, “Early Pregnancy Loss,” Practice Bulletin, no. 200 (November 2018): 197–207, https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2018/11/early-pregnancy-loss.
[4] Ibid., 198.
[5] Ibid., 199.
[6] Ibid., 201.
[7] Ibid., 203.
[8] “Risk Evaluation and Mitigation Strategy (REMS),” REMS Approved in 2016, U.S. Food & Drug Administration, accessed October 31, 2023, https://www.fda.gov/media/164649/download.
[9] Sheila Desai, Rachel K Jones, and Kate Castle, “Estimating abortion provision and abortion referrals among United States obstetrician-gynecologists in private practice,” Contraception 97, no. 4 (April 2018): 297-302, doi: 10.1016/j.contraception.2017.11.004; Debra B. Stulberg, et al., “Abortion Provision Among Practicing Obstetrician-Gynecologists,” Obstet Gynecol. 118, no. 3 (September 2011): 609-614, doi: 10.1097/AOG.0b013e31822ad973.
[10] Justin J Chu, et al., “Mifepristone and misoprostol versus misoprostol alone for the management of missed miscarriage (MifeMiso): a randomised, double-blind, placebo-controlled trial,” Lancet 396, no. 10253 (September 2020): 770-778, doi: 10.1016/S0140-6736(20)31788-8.
[11] Jay Ghosh, et al., “Methods for managing miscarriage: a network meta-analysis,” Cochrane Database Syst Rev. 6, no. 6 (June 2021): CD012602, doi: 10.1002/14651858.CD012602.pub2.