The Effect of Legalizing Assisted Suicide on Palliative Care and Suicide Rates: A Response to Compassion and Choices
This is Issue 13 of the On Point Series.
Introduction
The leading national organization promoting legalization of physician-assisted suicide, “Compassion & Choices” (formerly known as the Hemlock Society), has distributed a December 2016 “Medical Aid in Dying Fact Sheet” in various state legislatures around the country to persuade them to approve what they call “medical aid in dying.” This involves authorizing physicians to prescribe lethal overdoses of barbiturates to patients they diagnose as having six months or less to live, so the patients may use them to cause their own deaths. The flagship law in this agenda is an Oregon law approved by the state’s voters in 1994, which took effect late in 1997. C&C claims, among other things, that two decades of experience in Oregon show that legalization leads to improvements in palliative and end-of-life care and reduces “violent” suicides, and it cites articles in medical journals that it says support this claim. In fact, the medical literature, far from lending support to C&C’s agenda, underscores the adverse effects of that agenda to vulnerable people generally and to seriously ill patients in particular.
The “Compassion & Choices” (C&C) claim that legalizing assisted suicide improves palliative and end-of-life care: A response
C&C has circulated a “Medical Aid in Dying Fact Sheet” in state legislatures, claiming that “almost two decades” of experience in Oregon show improvements in palliative care due to the state’s legalization of physician-assisted suicide. Here are the claims, with a response.
Claim:
“End-of-life care has improved overall since the law’s implementation, in large part due to the dialogue the Death with Dignity Act encourages between people and their doctors.”
Facts:
The article cited for this broad claim, from the Journal of Palliative Medicine, doesn’t show this. It specifically studied only “hospice utilization rates” across the country at one particular time, in 2011. Oregon fared well in the survey – it was a leader in palliative care among the states before legalization—but in some ways other states fared better (see response to next claim below). This article says only that “it is possible” that the state’s assisted suicide law “has resulted in or at least reflects” more attention to end-of-life care.[1]
Even that article’s tentative suggestion was shown to be misleading when experts reviewed its hospice utilization data. In fact, Oregon’s major improvements in hospice care long predate passage of the “aid in dying” law; after legalization, its percentage improvement in hospice utilization fell below the national average, and it opened only five new hospices while 1,832 were opening in other states. Other states that have legalized physician-assisted suicide, such as Washington and Vermont, have a hospice utilization rate below the national average.[2]
As for end-of-life care improving “overall” due to legalization, findings published in the very journal cited by C&C suggest that the opposite occurred after the law took effect:
“The frequency of family reports of moderate or severe pain or distress in Oregon decedents increased – from 30.8% in 1996-1997 to 48% in 1999-2002 … represent[ing] the increased suffering of over 5,000 additional decedents and families. Higher levels of pain have profound effects on seriously ill patients and are associated with greater functional impairment, greater depression, anxiety and suicidal ideation, and worsening cognition…. Medicare patients in Oregon have among the lowest reimbursement in the United States during the last six months of life and have fallen significantly during the study period.”[3]
The Oregon Public Health Division’s “Death with Dignity Act” reports show that 90% of patients ingesting the lethal medication are enrolled in hospice. Yet from 1998 to 2015, 26% of the patients said they were ending their lives due to “inadequate pain control or concern about it”; 35% gave this reason in 2016. This does not suggest that Oregon hospice care is improving its ability to address all cases of pain in terminally ill patients.[4]
Consistently, palliative care has improved markedly when states (including Maryland in 1999) passed laws that prohibit assisted suicide but explicitly allow use of powerful and effective drugs like morphine to control pain. According to a palliative care expert at Johns Hopkins University School of Medicine, “in Maryland as well as in every state that had passed such legislation, there was an increase in the legitimate prescription of opioids and other strong medications used for pain control. Indeed, physicians universally expressed a mixture of relief and elation on knowing that, for the first time, such protective legislation existed.”[5]
By contrast, after Oregon’s assisted suicide law took effect, inpatient morphine use in the state “did not increase significantly for dying patients from 1997 to 1999.”[6] Again, this is from the same journal, and one of the same authors, cited by C&C.
In 2002 – eight years after the Oregon law was approved, and four years after it had taken effect – a nationwide study by the respected Last Acts coalition, funded by the Robert Wood Johnson Foundation, “graded” the 50 states on various elements of palliative care. A number of states where assisted suicide is illegal outpaced Oregon in key areas. On median number of days in hospice, Oregon received a “D” (six states had a better grade); on percentage of hospitals reporting a pain management program, a C (five states and the District of Columbia were better); on percentage of hospitals reporting a hospice program, a D (three states); on percentage of hospitals reporting a palliative care program, an E (11 states and the District of Columbia); on percentage of nursing home residents with persistent pain, a C (one state, Hawaii, had a better grade; only 11 states had a worse one); on strength of the state’s pain policies, a C (16 states better); on percentage of primary care physicians who are certified in palliative medicine, a C (14 states); on percentage of nurses certified in palliative care, a B (5 states). The study noted that 30 states had statewide coalitions or partnerships to improve care of the dying; Oregon was not among them.[7]
Claim:
“Hospice use is high and referrals are up, as is other use of palliative care.”
Facts:
This claim again cites only the 2015 hospice utilization study (note 1 above). That study did not report on “other use of palliative care,” and did not show referrals are “up” – it was a snapshot of the 50 states in one year, 2011. As for hospice use being “high”: In 2011, the percentage of dying patients that use hospice was an average of 47% nationwide, and highest in Utah (61%). The problem of “very short hospice enrollment” was least severe in the District of Columbia; the problem of “very long hospice enrollment” was least severe in Connecticut; and hospice disenrollment (people leaving hospice before death) was lowest in Hawaii. In 2011, none of these jurisdictions, which outranked Oregon in key areas, had legalized physician-assisted suicide.
Vermont legalized physician-assisted suicide in 2013. In 2015, the state’s Visiting Nurse Association announced it is conducting a study to discover why the state has “the third lowest hospice utilization rate in the nation.”[8]
Claim:
“Some hospice programs in Oregon reported a 20 percent increase in referrals since the medical aid in dying was authorized.”
Facts:
The only source cited here is an article in the Annals of Internal Medicine from January 1996, almost two years before the new law took effect. The very different and negative impact once the law actually took effect near the end of 1997 is documented above (notes 2, 3 and 6).[9]
There are many proven ways to increase hospice referrals without dispensing deadly drug overdoses to patients. In St. Mary’s County, Maryland, for example, a simple “community outreach” to educate local physicians about hospice care resulted in a greater than 50% increase in average utilization of the county’s hospice over three months; from the beginning of the three-month period to its end, enrolled patients increased over 150% (from 21 to 54).[10]
Claim:
“In-hospital death rates are the lowest in the nation and at-home death rates are the highest in the nation, and violent suicide among hospice patients has virtually disappeared.”
Facts:
The only source cited here says nothing to document this claim. It is an article posted on C&C’s web site, written by a group convened by C&C itself to promote “clinical criteria” for the “aid in dying” process. Some of the criteria, if implemented, would violate even the Oregon law – for example, they say a second opinion by another physician should not be required.[11]
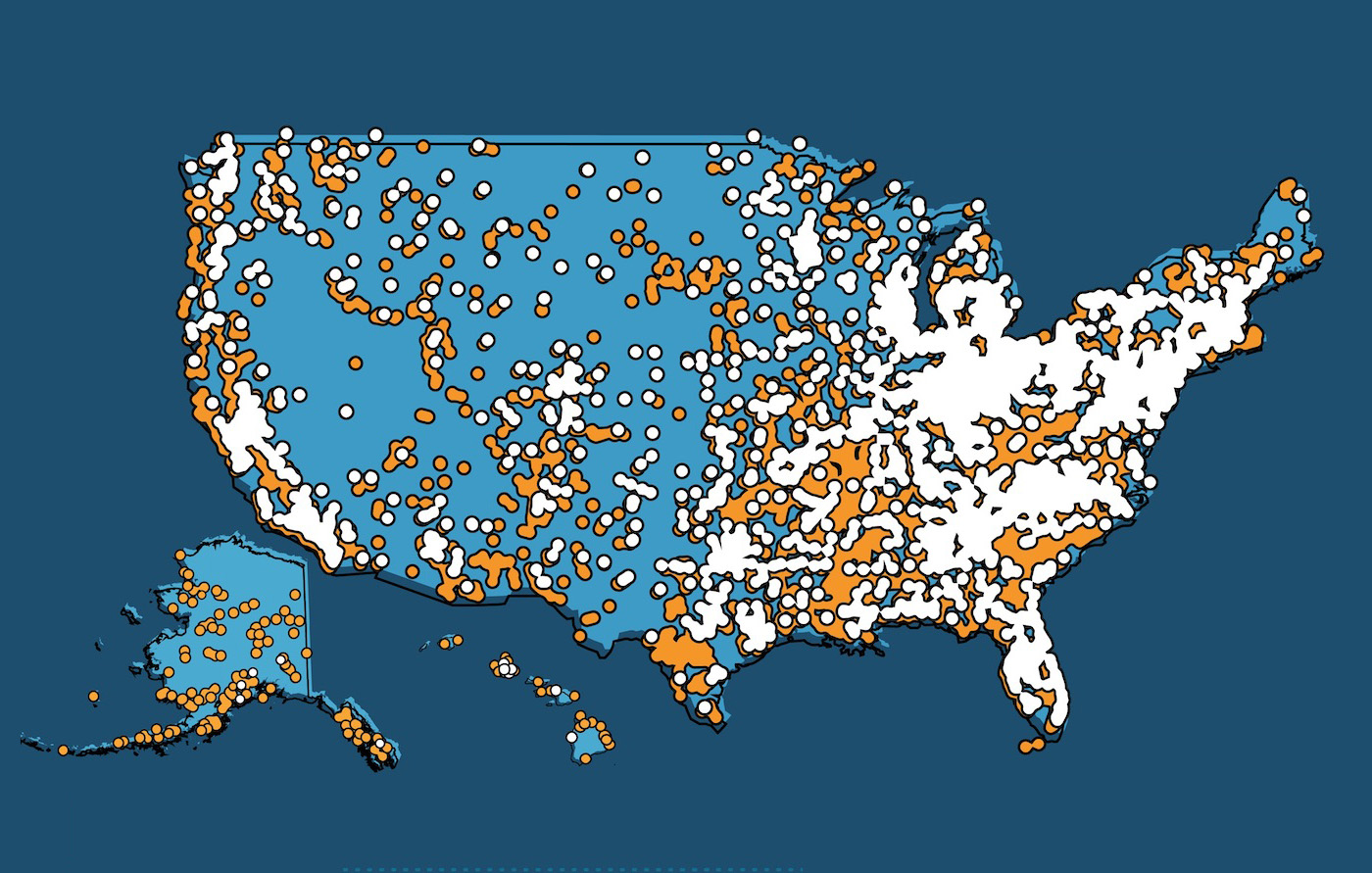
There is documentation, however, on overall suicides in Oregon. According to the U.S. Centers for Disease Control and Prevention, Oregon’s suicide rate increased 49% between 1999 and 2010 (compared to 28% nationally). Oregon’s own health department says the state’s suicide rate has been rising since 2000 and, as of 2012, was 42% higher than the national average.[12] These figures are in addition to cases of “aid in dying,” which Oregon law forbids counting as suicides.
A recent scholarly study concluded that legalizing assisted suicide does not reduce or substitute for more “violent” suicides but increases total suicides.[13]
It is also well known that favorable publicity about suicide and assisted suicide leads to “imitative suicidal behaviors,” especially among young or depressed people. The World Health Organization warns news media: “Avoid language which sensationalizes or normalizes suicide, or presents it as a solution to problems”; “Avoid explicit description of the method used in a completed or attempted suicide.”[14] Through its celebration of assisted suicide as a solution to seriously ill patients’ problems, and its “clinical criteria” detailing how to take a lethal drug overdose, C&C’s campaign violates all these rules.
Conclusions
- The studies cited by C&C generally do not show what it claims, and their conclusions have been corrected or modified by other studies.
- There is no convincing evidence that laws allowing physician-assisted suicide improve palliative and end-of-life care, and there is significant evidence that such laws can have the opposite effect – and that the laws, and the campaign promoting them, have a disturbing impact on overall suicide rates.
- If these laws have a deleterious effect on palliative and end-of-life care, and on suicide prevention efforts, in the general population of the states enacting them, the number of people (including seriously ill people) adversely affected by them vastly exceeds the number of patients who actually make use of the “aid in dying” option.
Richard M. Doerflinger, M.A. is an associate scholar with the Charlotte Lozier Institute. He wishes to express his appreciation to Jennifer Ballentine, President of The Iris Project, for assistance in understanding recent developments in palliative and end-of-life care.
[1] S. Wang et al., “Geographic variation of hospice use patterns at the end of life,” Journal of Palliative Medicine 18 (2015): 771–780 at 778 (emphasis added).
[2] J. Ballentine et al., “Physician-Assisted Death Does Not Improve End-of-Life Care,” Journal of Palliative Medicine 19 (2016): 1-2.
[3] E. Fromme et al., “Increased Family Reports of Pain or Distress in Dying Oregonians: 1996 to 2002,” Journal of Palliative Medicine 7 (2004): 431-42 at 437, 439.
[4] Oregon Public Health Division, “Oregon Death with Dignity Act: Data summary 2016” at 9-10; http://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year19.pdf.
[5] F. Michael Gloth, III, M.D., F.A.C.P., Handbook of Pain Relief in Older Adults: An Evidence-Based Approach” (Humana Press 2004): 193. For data on the increased use of morphine for pain control in 12 states after they passed such laws, see Brief Amicus Curiae of the U.S. Conference of Catholic Bishops, et al., in Gonzales v. State of Oregon (May 9, 2005): 18-22, at http://www.usccb.org/about/general-counsel/amicus-briefs/upload/amicus-sct-gonzales-v-oregon-2005-05.pdf.
[6] S. Tolle, et al., “Trends in Opioid Use Over Time: 1997 to 1999,” 7 J. of Palliative Med. 39 (2004).
[7] Last Acts, Means to a Better End: A Report on Dying in America Today (November 2002): 19, 23, 24, 25, 32, 36, 41, 42, 55.
[8] “Vermont VNA Seeking to Identify Causes of State’s Low Hospice Utilization Rates,” Hospice and Palliative Care News, April 29, 2015, at http://healthrespubs.com/hospice-and-palliative-care-news/2015/04/29/vermont-vna-seeking-to-identify-low-hospice-utilization-rates/.
[9] The Oregon law was approved by voters in November 1994 but enjoined by a federal court that initially found constitutional problems; that ruling was overturned by an appellate court. Then implementation was delayed while a new ballot initiative to rescind the law was considered; that initiative failed in November 1997. The first full year the law was in effect was 1998.
[10] C. Taylor, “Improving Referral of Patients to Hospice Through Community Physician Outreach,” 28 Journal of Pain and Symptom Management (2004): 294-5.
[11] D. Orentlicher, et al., “Clinical Criteria for Physician Aid in Dying,” Journal of Palliative Medicine 19 (2016): 259-62 at 260. (C&C’s citation suggesting 2015 publication refers to an advance online version now superceded.)
[12] X. Shen and L. Millet, Suicides in Oregon: Trends and Associated Factors. 2003-2012 (Oregon Health Authority 2015); http://public.health.oregon.gov/DiseasesConditions/InjuryFatalityData/Documents/NVDRS/Suicide%20in%20Oregon%202015%20report.pdf.
[13] D. Jones and D. Paton, “How Does Legalization of Physician-Assisted Suicide Affect Rates of Suicide?”, Southern Medical Journal 108 (2015): 599-604.
[14] World Health Organization, Preventing Suicide: A Resource for Media Professionals (WHO: Geneva 2008): 6, 7, 8; www.who.int/mental_health/prevention/suicide/resource_media.pdf. Similar guidelines have been issued by public health and suicide prevention organizations in the United States, and endorsed by the U.S. Surgeon General. See http://reportingonsuicide.org/ and https://www.surgeongeneral.gov/library/reports/national-strategy-suicide-prevention/full_report-rev.pdf.