Immediate Physical Complications of Induced Abortion
This is Issue 11 of the On Science Series.
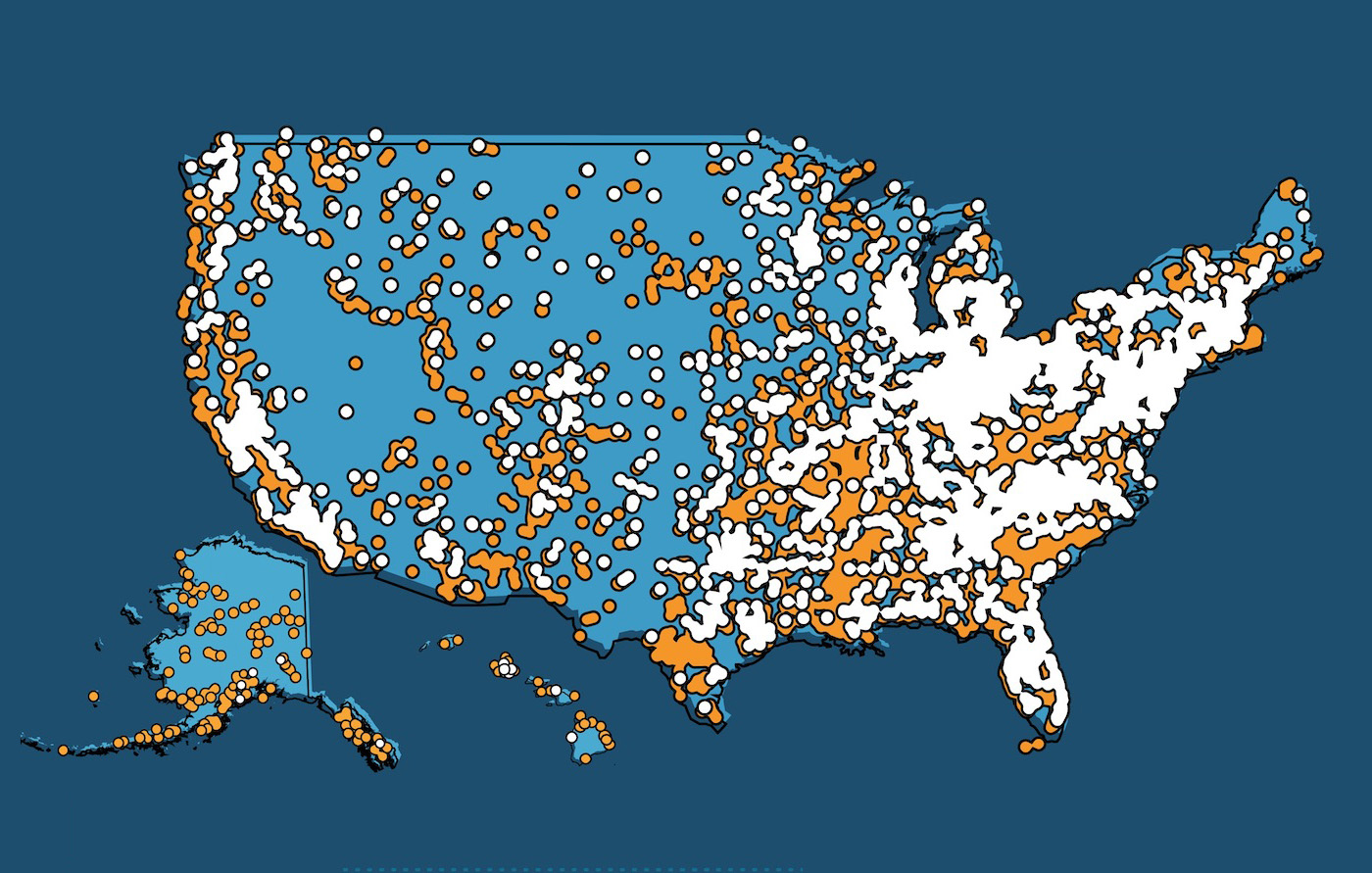
Researchers associated with the abortion industry and their media advocates promote induced abortion by stating it is safer than Tylenol, penicillin, or Viagra.[1] These dangerously misleading statements ignore the numerous data deficiencies of abortion-complication reporting in the U.S. There is no federal mandate for reporting of abortion numbers, complications or deaths associated with induced surgical or chemical abortion; the U.S. Centers for Disease Control and Prevention (CDC) data on abortion rests solely on voluntary reporting by the states’ health departments. This leaves significant gaps in the public health data.[2]
Since most abortions are paid for privately, it is difficult to link abortion procedures with insurance payments for complications through records-linkage studies. Although some states have mandated reporting of abortion complications, there are few enforcement mechanisms in effect, allowing the abortion industry to choose whether to report complications from their procedures.[3] To reach accurate conclusions regarding physical complications following abortion, an observer must view the abortion industry’s claims with skepticism and seek additional information to find the truth.
Complications in Early Abortions:
Possible physical complications after first trimester surgical abortions, as discussed below:
- Hemorrhage
- Infection
- Retained pregnancy tissue
- Cervical damage, possible cervical incompetence leading to future premature delivery
- Damage to lining of uterus, possible abnormal placental attachment in the future pregnancies
- Uterine perforation or rupture
- Injuries to surrounding organs
- Anesthetic reactions or complications
- Failure to end the life of the embryo/fetus
- Death
First, one must become aware of the details of abortion procedures to understand ways that complications can occur. A surgical first-trimester abortion is usually performed by uterine aspiration (also known as dilation and suction aspiration and/or curettage; D&C), which appears to have low complication rates when performed by experienced surgeons. A 2015 Planned Parenthood study reported 0.7% complications after early surgical abortions, but the reported “loss-to-follow-up rate” was 16.9%, documenting a common problem in studies of abortion complications – unknown outcomes of many abortions. The unwarranted assumption is usually made that women who do not return have had uncomplicated abortions.[4]
In a 2013 study, Planned Parenthood, analyzing their clinic charts, documented significant adverse events following only 0.16% of chemical abortions.[5] This completely ignores the reality that women experiencing significant adverse events, such as hospital admission, blood transfusion, emergency department treatment, intravenous antibiotics, infection and death, would be treated in a hospital, and would not return to the abortion clinic. Since most abortionists do not maintain hospital privileges, these injured women would be cared for by other physicians.[6] Another 2015 abortion industry study reported only 0.87% of abortions resulted in complications treated in the emergency room, but these numbers were achieved by ignoring ICD coding deficiencies and limiting inclusion to very few specific codes.[7] In contrast, a more thorough records-linkage study by independent investigators documented that in 2015, 6% of women presented to an emergency room with chemical abortion-related complications and 4% presented with surgical abortion-related complications in the month following their abortion.[8]
A uterine aspiration abortion procedure begins with placement of a speculum for visualization of the cervix, which is grasped with a sharp tenaculum, which can lacerate the cervix. Sometimes a prostaglandin such as misoprostol has been placed a few hours in advance to soften the cervix to facilitate dilatation. An anesthetic is generally injected into the cervix to reduce pain, but if inadvertently injected into the bloodstream it can cause seizures. Similarly, intravenous pain or anxiolytic medication can be given, but must be closely supervised to prevent overdose or anesthetic reactions. The cervix is then mechanically dilated with progressively enlarging metal dilators to allow introduction of instruments. The strong, healthy cervix may be resistant to the dilatation because it is designed to remain closed until natural childbirth, and inadvertent creation of a false passage can occur. Additionally, cervical damage may lead to scarring or damage to the musculature, which could result in infertility from cervical stenosis or future pregnancy complications such as incompetent cervix leading to preterm rupture of membranes and early delivery.[9]
Once the uterus is entered, a suction curette is introduced, and powerful suction is created through an electric vacuum aspiration machine. Manual vacuum aspirators are sometimes used in geographic areas without adequate electricity, but suction may not be as strong, predisposing to retained tissue in the uterus. The suction is used to remove the embryo/fetus, placenta and amniotic fluid. A sharp curette may be introduced to scrape along the uterine walls to ensure all the tissue has been removed, although if this is performed too aggressively it may result in damage to the uterine walls, leading to a potentially dangerous delivery from abnormal placental adherence in a subsequent pregnancy.[10] The abortionist should examine the aspirated tissue to ensure the pregnancy has been completely removed, as retained tissue can lead to infection, hemorrhage and future infertility from scar tissue or future pregnancy complications if a pregnancy occurs. Additionally, confirmation of intrauterine pregnancy tissue provides reassurance that the pregnancy was not implanted in an extrauterine location, as failure to diagnosis ectopic pregnancies sometimes leads to internal hemorrhage and death in women undergoing abortion.[11]
Any abortion can result in complications, particularly if performed by a poorly skilled or otherwise compromised abortionist. Many abortion providers operate outside of the supervision of organizations such as Planned Parenthood or the National Abortion Federation,[12] and the political nature of abortion makes it unlikely that local health departments provide oversight unless reports of egregious violations of standard practice occur. This reality was recently demonstrated in Pensacola, Florida, where an emergency suspension order was issued against the Integrity Medical Care abortion clinic. The clinic was closed due to the Florida Agency for Health Care Administration’s finding that the clinic posed an “immediate serious danger to the public health.”[13] One patient presented on March 23, 2022, for an abortion at 20 weeks, 2 days gestation, whose procedure was complicated by bleeding. She was transferred to a local hospital where her pulse was undetectable, and she was responsive only to painful stimuli. She required an emergency hysterectomy for a ruptured uterus. Another patient presented on May 5, 2022, for an abortion at 19 weeks, 6 days gestation. Her uterus was perforated during the procedure, causing her to bleed. She remained unmonitored for six hours, after which her husband was directed to take her to an emergency room across state lines (which presumably would not report the complication to Florida as mandated). On arrival, she was “hemodynamically unstable” and required a “mass transfusion protocol to replace egregious blood loss.” When news was released that a third woman had been similarly seriously injured by the same provider, the abortionist’s medical license was finally suspended.[14]
Common minor complications of surgical abortions include bleeding, which may require medication or additional surgery; infection, which may require oral or intravenous antibiotics; incomplete tissue removal, which may require an additional surgical procedure; as well as side effects from anesthesia or anxiety related to the procedure. More serious complications may occur due to misdirection of cervical dilators or accidental insertion of suction curettes or grasping forceps into the soft, gravid uterus, which may perforate the uterus, potentially causing injury to adjacent major blood vessels and/or gynecologic, genitourinary or gastrointestinal organs, which may require blood transfusion and/or emergency abdominal surgical exploration to perform a hysterectomy, bowel resection, bladder repair, or other repairs.[15] Death can occur due to hemorrhage (resulting in hemodynamic instability from blood loss), sepsis (system-wide infection), thrombotic emboli (blood clots obstructing vessels), intravascular amniotic or air emboli (debris in the bloodstream), serious complications of anesthesia and cardiac or cerebrovascular events.[16]
Alternatively, a medical, or chemical, abortion may be induced with two drugs. Mifepristone (Mifeprex or RU-486) blocks progesterone receptors to cut off hormonal support for the pregnancy, resulting in disruption of the implantation site and fetal death. Misoprostol (Cytotec) is consumed 24-48 hours later to induce contractions to expel the dead embryo/fetus and placental tissue.[17] This regimen is approved by the FDA until 10 weeks gestational age,[18] but some abortion providers ignore this and prescribe the drug a week later or more.[19] In 2020, 54% of reported abortions in the U.S. were induced by these drugs.[20]
Possible physical complications after first trimester chemical abortions, as discussed below:
- Hemorrhage
- Infection, possible sepsis
- Retained pregnancy tissue
- Need for surgical completion, with surgical risks as documented above
- Failure to end the life of the embryo/fetus
- Rh isoimmunization if Rhogam not given if indicated
- Ruptured ectopic pregnancy if undiagnosed
- Death
Women often choose this method under the assumption that it is safer and more natural, yet complications occur four times more frequently from chemical than from surgical abortions.[21] The average woman bleeds for 9-16 days and 8% will bleed longer than a month.[22] At least 1% will require hospitalization for hemorrhage or infection, 1% will have ongoing viable pregnancies (the drugs will fail to kill the fetus), and surgery for incomplete abortion will be required in 3.4-7.9%.[23] If a pregnancy continues to birth, teratogenic effects from misoprostol causing birth defects such as clubfoot, cranial nerve anomalies and limb abnormalities are sometimes seen.[24] The side effects of cramping, vaginal bleeding, hemorrhage, nausea, weakness, fever, chills, vomiting, headache, diarrhea, and dizziness occur in almost all women.[25]
Recent research suggests that mifepristone itself may also cause complications of hemorrhage, infection, and mental health issues through direct pharmacologic effects. Mifepristone impairs the ability of the spiral arterioles in the uterus to contract, predisposing to excessive blood loss.[26] It also blocks glucocorticoid receptors which may contribute to an impaired inflammatory response, increasing the risk of infection. Misoprostol also suppresses the immune system, and if dead tissue is retained, that will also predispose the woman to infection.[27] Twenty-four deaths have been reported to the Food and Drug Administration (FDA) after chemical abortion, seven related to infection by a common organism, clostridium sordelii, which is easily combatted in a healthy immune system.[28] In addition, mifepristone releases inflammatory cytokines which have been implicated in causing depression. In a rat model the mifepristone termination group had significantly decreased body weight, food intake, locomotor-related activity, and sucrose consumption, which are all animal proxies for depression and anxiety in humans.[29] It has been extensively documented that the chemical abortion complications reported by the FDA consist of only a small percentage of the total complications due to incomplete reporting and frequent misattribution of chemical abortion complications to miscarriages.[30]
In December 2021, the FDA removed its Risk Evaluation and Mitigation Strategy (REMS) in-person prescribing requirements, allowing mifepristone provision without sonogram or exam (needed to document gestational age or intrauterine vs. ectopic pregnancy),[31] or without labs (needed to document blood Rh status and provision of Rhogam if indicated to prevent isoimmunization).[32] This change allows telemedicine prescribing, internet ordering and mail order provision of these dangerous drugs. This will undoubtedly increase the risk of failures and adverse events after chemical abortions.[33] Additionally, it may encourage coercion of hesitant women by unwilling partners, incestuous abusers and sex traffickers into unwanted abortions.[34]
Mifepristone and misoprostol have no action on an ectopic pregnancy because these medications exert their actions on the uterus, allowing the pregnancy to continue to grow, possibly to the point of tubal rupture which can lead to catastrophic bleeding and death. It has been documented that a woman is 30% more likely to die from a ruptured ectopic while seeking abortion if it remains undiagnosed, because she may interpret the warning signs of pain and bleeding as signs the chemical abortion pills are working rather than a warning sign that her life is in danger.[35] While ectopic implantations occur in only 2% of pregnancies, they account for up to 10% of maternal deaths.[36] Half of women with ectopic pregnancies have no risk factors for this serious condition, and the gold standard for diagnosis is ultrasound.[37]
Complications in Later Abortions:
Possible physical complications after second or third trimester abortions, as discussed below:
- Hemorrhage
- Infection
- Retained pregnancy tissue
- Cervical damage, possible cervical incompetence leading to future premature delivery
- Damage to lining of uterus, possible abnormal placental attachment in future pregnancies
- Uterine perforation or rupture
- Injuries to surrounding organs
- Anesthetic reactions or complications
- Failure to end the fetal life, possible live birth
- Death
An abortion performed after the early second trimester (>13-14 weeks’ gestation) is more complicated and must be performed in one of the following ways: A Dilation and Extraction (D&X, non-intact D&E or “partial birth” abortion) can be performed by delivering the fetus as breech to the level of his head, then crushing his skull and removing brain tissue to assist removal, but this method is banned by federal law and by many states, when performed on a living fetus. Another rarely performed method is hysterotomy, which involves performing feticide to kill the baby and then performing a C-section to deliver the dead baby, but this procedure is used only in extraordinary circumstances when other abortion methods fail.[38] Likewise, a hysterectomy can be performed to remove the uterus and the unborn baby at the same time, such as treatment for reproductive tract malignancies.[39] These intraabdominal procedures have three times the risk of maternal mortality compared to D&E procedures and are used rarely.[40]
The most commonly performed later abortion method is Dilation and Evacuation (D&E or “dismemberment” abortion), accounting for about 95% of abortions after the early second trimester.[41] This procedure was vividly described by Supreme Court Justice Clarence Thomas in his dissenting opinion in the 2000 SCOTUS’ Stenberg v. Carhart ruling, quoting the words of the abortionists’ testimonies, “Because of the fetus’ size at this time, the physician generally removes the fetus by dismembering the fetus one piece at a time…The doctor grabs a fetal extremity, such as an arm or a leg, with forceps and pulls it through the cervical os…tearing…fetal parts from his body…by means of traction…The fetus will die from blood loss…When all of the fetus’ limbs have been removed, and only the head remains in-utero, the physician will then collapse the skull and remove it though the cervical canal. At the end of the procedure, the physician is left, in respondent’s words, ‘with a tray full of pieces.’”[42]
In a healthy pregnancy the cervix is strong and difficult to dilate, and thus cervical ripening (usually with a water-absorbing laminaria or prostaglandin medication) is performed for one to three days prior to the abortion. If dilation remains difficult, cervical damage can occur or a false channel can be created, possibly leading to laceration of cervical vessels or injury to adjacent organs such as bladder, ureter or bowel. Once dilation has been completed, the surgeon introduces a suction curette into the uterus to vacuum out amniotic fluid and soft tissue such as the placenta. At this late gestational age, the fetal bones are calcified, and must be removed in a piecemeal fashion with grasping clamps, hence the layman’s description “dismemberment abortion.” Multiple passes are required to remove all the fetal tissue, as each pass may yield an arm, leg or section of torso. Uterine lacerations may occur from fragments of sharp fetal bones. The cranium is often the most difficult portion of tissue to remove as it may require crushing to fit through the incompletely dilated cervix.
Complications which may occur with this operation include instrumental perforation of the soft, distended uterus, with injury to surrounding bowel or vasculature, potentially leading to sepsis or uncontrollable bleeding; or the incomplete removal of all the fetal tissue which may lead to hemorrhage, infection, chronic pain, or future infertility. Additional surgery may be needed to repair these damages.[43] Surgery can also cause uterine damage leading to future pregnancy complications such as abnormal placental attachment or premature labor. Severe complications can also lead to an abnormal activation of a woman’s blood clotting system, disseminated intravascular coagulation, which can lead to death from uncontrollable bleeding due to inability to create blood clots.[44]
Complications and maternal mortality associated with D&E procedures increase with gestational age, tripling the risk when D&E is performed at greater than 16 weeks when compared to 13-15 weeks’ gestation.[45] Beyond 21 weeks, around the cutoff for fetal viability, the risk of maternal mortality from D&E exceeds the risk from childbirth.[46] CDC data further documents that the risk of maternal mortality increases by 38% for each week an abortion is performed beyond eight weeks, reaching a 15-fold increase early in the second trimester, 30-fold increase in the mid-second trimester, and 76-fold increase after viability.[47] Similarly, another CDC study documented a 2.5-fold increase in mortality risk beyond 18 weeks’ gestation compared with an earlier D&E.[48]
Experience of the physician also impacts risk because D&E is a very complex procedure. This fact was acknowledged by the Accreditation Council for Graduate Medical Education (ACGME) when it introduced a two-year fellowship called Complex Family Planning to train physicians to perform this complicated procedure.[49] Whereas most high-volume abortionists report D&E complication rates of 1-7%,[50] resident physicians in training documented 11% major complications (death, prolonged hospitalization, transfusion, exploratory surgery, stroke, heart attack, pulmonary embolus, and deep venous thrombosis), and had 24% readmission rates.[51] Other studies document even higher complication rates: the University of California, San Francisco reported 13% complications/10% hemorrhage for treatment of late miscarriage with D&E, and 10% complications/7% hemorrhage from D&E on a living fetus.[52] Two other recent studies documented hemorrhage rates greater than 50% using standard D&E procedures.[53]
A sobering look at what these complications can look like can be obtained from the 1996 book, Lime 5: Exploited by Choice, where an investigative journalist documented abortion complications recorded in medical malpractice cases. He was able to document 39% more deaths from abortion than the CDC reported, even though women and their families are extremely unlikely to initiate a malpractice case following harm from abortion due to shame and stigma. Deficiencies in pre-operative counseling, abortionists compromised by poor skills or substance abuse, egregious violations in standard practice resulting in fatal complications, and inadequate postoperative recovery care were all shown to be common factors in these poor outcomes. Uterine rupture resulting in lacerated intestines, compromised ureters, even damaged kidneys (located far from the uterus in the mid-upper back) were all documented. As an example, the surgeon who performed a hysterectomy to save the life of one severely injured woman testified in court, “It would take a lot of force-an extreme amount of force-to do that kind of damage.” Regarding that case, the medical board stated that, “having nearly eviscerated his patient and with her clearly in critical condition, he sent her to the hospital in a private car during rush hours… A more egregious example of incompetence and gross negligence is difficult to imagine.”[54] Although this particular case happened years ago, the recent report of the Pensacola abortionist demonstrates that the unsupervised abortion profession continues to provide risky, substandard care.
As the fetus becomes bigger, D&E becomes harder to perform due to the difficulty in eviscerating and disarticulating the fetus, so the abortionist may choose to perform an induction abortion. Labor may be induced with prostaglandins such as misoprostol, with or without mifepristone, intravenous pitocin or rarely, saline, urea or prostaglandin intraamniotic infusion.[55] Infection, hemorrhage or retained tissue often require a surgical suction and/or sharp curettage afterward to treat these complications, affecting 5-39% of women.[56] Saline can also cause life-threatening electrolyte imbalances and prostaglandin infusion is associated with life-threatening sepsis, so they are rarely performed today.[57]
“The dreaded complication” of later labor inductions, the birth of a live baby, is rarely discussed, but may occur more frequently than acknowledged. European studies have documented that more than half of anomalous fetuses aborted between 20-24 weeks will survive the induction if feticide is not performed first.[58] There are several available methods by which the abortionist can kill the fetus before labor induction, although a recent survey of abortion providers demonstrated that 69% of abortion providers do not routinely provide feticide after 18-weeks’ gestation.[59] Feticide may occur by umbilical cord transection early in the procedure but may also involve fetal intraamniotic or intracardiac potassium chloride or digoxin injection which can entail additional risks to the woman if these potent cardiotoxic medications should enter her bloodstream.[60] A vocal abortion advocate advises against feticide, stating that women who request it are responding to misinformation, and are “inappropriately concerned about the potential for fetal pain, a biologic impossibility at these gestational ages.”[61] By making this statement, he demonstrated either his ignorance of the recent literature or his pro-abortion bias because leaders in the field of fetal pain research, regardless of their personal views, have argued that fetal pain is possible as early as 12 weeks and should be considered in the discussion surrounding abortion.[62]
Operation Rescue, an abortion watchdog organization, documented 129 facilities that performed abortions after 20 weeks’ gestation in 2019. This included several that perform the procedure in the third trimester: Boulder Abortion Clinic run by Dr. Warren Hern that advertises no gestational age limits, Capital Women’s Services in D.C. run by Dr. Steven Chase Brigham with a 36-week limit, CARE in Bethesda, MD run by Dr. LeRoy Carhart with a 35-week limit, Southwestern Women’s Options in Albuquerque run by Dr. Curtis Boyd with no limits, and DuPont Clinic in D.C. which also has no limits on the gestational age at which they will perform an abortion.[63]
Deaths following abortion:
Possible physical complications leading to death after any abortion:
- Hemorrhage leading to hypovolemic shock, disseminated intravascular coagulation
- Infection leading to sepsis
- Future premature delivery leading to magnesium sulfate toxicity or complications from other interventions
- Future abnormal placental attachment leading to catastrophic hemorrhage
- Uterine perforation or rupture leading to injuries to surrounding organs
- Anesthetic reactions, complications or overdose
- Thrombotic, amniotic or septic emboli
- Above complications can lead to stroke, cardiovascular collapse
As discussed previously, the CDC’s maternal and abortion-related mortality data is notoriously incomplete. Such incomplete U.S. data appears to document fewer deaths after abortion than after childbirth,[64] but higher-quality international records-linkage studies document the opposite result. When linking all death certificates of reproductive aged women to all pregnancy outcomes, studies in Finland and Denmark and on California Medicaid recipients have all documented a much higher likelihood of death in the year following an induced abortion than following term childbirth.[65] Specifically, in Finland, deaths from all causes after abortion were two to four times as frequent as following childbirth. The risk of death from any violent cause was six times higher after abortion than childbirth, suicide six times higher, accidental death five times higher, and death by homicide 10 times higher.[66] These comprehensive Finnish records-linkage studies also demonstrate that death certificate documentation alone detects only 26% of deaths after live birth or stillbirth, 12% of deaths following miscarriage or ectopic pregnancy, and just 1% of deaths following induced abortion.[67] The above discussion documents a vivid picture of how death from an immediate physical complication may occur after abortion.[68]
Ingrid Skop, M.D., F.A.C.O.G., is Senior Fellow and Director of Medical Affairs at Charlotte Lozier Institute.
[1] “Analysis of Medication Abortion Risk and the FDA Report ‘Mifepristone U.S. Post-Marketing Adverse Events Summary Through 12/31/2018,’” Advancing New Standards in Reproductive Health, April 2019, accessed September 27, 2022, https://www.ansirh.org/sites/default/files/publications/files/mifepristone_safety_4-23-2019.pdf; “The Abortion Pill is Safer than Tylenol and Almost Impossible to get,” Bloomberg News, February 17, 2022, accessed September 27, 2022, https://www.bloomberg.com/news/features/2022-02-17/abortion-pill-mifepristone-is-safer-than-tylenol-and-almost-impossible-to-get.
[2] Chuck Donovan and Rebecca Gonzales, “Abortion Reporting: Toward a Better National Standard,” Charlotte Lozier Institute, August 24, 2016, accessed November 9, 2022, https://lozierinstitute.org/abortion-reporting-toward-a-better-national-standard-summary/; Tessa Longbons, “U.S. Abortion Trends: 2019 and Preliminary 2020,” Charlotte Lozier Institute, September 10, 2021, accessed November 9, 2022, https://lozierinstitute.org/us-abortion-trends-2019-and-preliminary-2020/.
[3] James Studnicki et al., “Improving Maternal Mortality: Comprehensive Reporting for All Pregnancy Outcomes,” Open Journal of Preventive Medicine 7, (2017): 162–181; Patrick Marmion and Ingrid Skop, “Induced abortion and the Increased Risk of Maternal Mortality,” The Linacre Quarterly 87, no. 3 (2020): 302-310,
[4] Luu Doan Ireland, Mary Gatter, Angela Chen, “Medical Compared with Surgical Abortion for Effective Pregnancy Termination in the First Trimester,” Obstetrics and Gynecology 126, (2015): 22-28, doi: 10.1097/AOG.0000000000000910.
[5] Kelly Cleland et al., “Significant Adverse Events and Outcomes After Medical Abortion,” Obstetrics and Gynecology 121, (2013): 167-171, doi: 10.1097/aog.0b013e3182755763.
[6] James Studnicki et al., “Doctors who Perform Abortions: Their Characteristics and Patterns of Holding and Using Hospital Admitting Privileges,” Health Services Research and Managerial Epidemiology 6, (2019): 1-8, doi: 10.1177/2333392819841211.
[7] Ushma Upadhyay et al., “Incidence of Emergency Department Visits and Complications After Abortion,” Obstetrics and Gynecology 125, (2015): 175-83, doi: 10.1097/AOG.0000000000000603.
[8] James Studnicki et al., “A Longitudinal Cohort Study of Emergency Room Utilization Following Mifepristone Chemical and Surgical Abortions, 1999-2015,” Health Services Research and Managerial Epidemiology 8, (2021): 1-8, 10.1177/23333928211053965.
[9] Hanes Swingle et al., “Abortion and the Risk of Subsequent Preterm Birth: A Systematic Review and Meta-Analysis,” Journal of Reproductive Medicine 54, (2009): 95-108; Hua Liao et al., “Repeated Medical Abortions and the Risk of Preterm Birth in the Subsequent Pregnancy,” Archives of Gynecology and Obstetrics 284, no. 3 (2011): 579-586; American Association of Pro-Life Obstetricians & Gynecologists, “The Association Between Surgical Abortion and Pre-Term Birth: An Overview,” AAPLOG Practice Guideline No. 5, last updated November 2021, accessed August 7, 2022, https://aaplog.org/wp-content/uploads/2021/11/PB-5-Overview-of-Abortion-and-PTB.pdf; American Association of Pro-Life Obstetricians & Gynecologists, “A Detailed Examination of the Data Between Surgical Abortion and Pre-Term Birth,” AAPLOG Practice Guideline No. 11, November 2021, accessed August 9, 2022, https://aaplog.org/wp-content/uploads/2021/11/PG-11-A-Detailed-Examination-of-the-Data-on-Surgical-Abortion-and-Preterm-Birth.pdf.
[10] Heather Baldwin et al., “Antecedents of Abnormally Invasive Placenta in Primiparous Women: Risk Associated With Gynecologic Procedures,” Obstetrics and Gynecology 131, no. 2 (2018): 227-233, doi: 10.1097/AOG.0000000000002434; Mulubrhan Mogos et al., “Recent Trends in Placenta Accreta in the United States and Its Impact on Maternal-Fetal Morbidity and Healthcare-associated Costs, 1998-2011,” Journal of Maternal-Fetal and Neonatal Medicine 29, no. 7 (2016): 1077, doi: 10.3109/14767058.2015.1034103.
[11] Grace Shih and Robin Wallace, “Up to date: First-Trimester Pregnancy Termination: Uterine Aspiration,” UpToDate, accessed September 27, 2022, https://www.uptodate.com/contents/first-trimester-pregnancy-termination-uterine-aspiration?topicRef=3313&source=see_link.
[12] “Why Become a NAF Member,” National Abortion Federation, https://prochoice.org/naf-membership/.
[13] Agency for Health Care Administration v. Integrity Medical Care, Emergency Suspension Order, May 20, 2022, https://apps.ahca.myflorida.com/dm_web/DMWeb_DocsFO/12267282.pdf
[14] Steve Warren, “Florida Suspends Medical License of Abortionist After Three Women Injured, Citing ‘no gynecologic surgical training,’” CBN News, August 5, 2022, accessed September 27, 2022, https://www1.cbn.com/cbnnews/2022/august/fl-suspends-medical-license-of-abortionist-after-3-women-injured-citing-no-gynecological-surgical-training.
[15] Maarit Niinimaki et al., “Immediate Complications After Medical Compared with Surgical Termination of Pregnancy,” Obstetrics and Gynecology 114, no. 4 (2009): 795-804, doi: 10.1097/AOG.0b013e3181b5ccf9; Amy Autry et al., “A Comparison of Medical Induction and Dilation and Evacuation for Second Trimester Abortion,” American Journal of Obstetrics and Gynecology 187, no. 2 (2002): 393-397; Willard Cates Jr. and Daniel Grimes, “Deaths from Second Trimester Abortion by Dilation and Evacuation: Causes, Prevention, Facilities,” Obstetrics and Gynecology 58, no. 4 (1981): 401-408.
[16] Gary Cunningham, Williams Obstetrics (Norwalk, CT: Appleton & Lange, 1993), 81-246; Sujata Lalitkumar, Marc Bygdeman, Kristina Gemzell-Danielsson, “Mid-trimester Induced Abortion: A Review,” Human Reproduction Update 13, no. 1 (2007): 37-52.
[17] Irving Spitz et al., “Early Pregnancy Termination with Mifepristone and Misoprostol in the United States,” The New England Journal of Medicine 338, no. 18 (1998): 1241-1247.
[18] “Mifeprex (Mifepristone) Information,” U.S. Food and Drug Administration (FDA), last modified December 16, 2021, accessed September 22, 2022, https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/mifeprex-mifepristone-information.
[19] “The Abortion Pill,” Planned Parenthood, accessed September 22, 2022, https://www.plannedparenthood.org/learn/abortion/the-abortion-pill. The article notes, “depending on where you live, you may be able to get a medication abortion up to 77 days (11 weeks) after the first day of your last period.” Also, Planned Parenthood’s Find a Health Center notes the locations of its abortion centers that offer chemical abortion pills up to 11 weeks.
[20] Rachel Jones et al., “Medication Abortion Now Accounts for More Than Half of all US Abortions,” Guttmacher Institute, February 2022, accessed September 26, 2022, Available at: https://www.guttmacher.org/article/2022/02/medication-abortion-now-accounts-more-half-all-us-abortions.
[21] Niinimaki et al., Immediate Complications, 795-804; Ireland et al., “Medical Compared with Surgical Abortion,” 22-28.
[22] “Mifeprex (Mifepristone) Information.” FDA.
[23] Elizabeth Raymond et al., “First Trimester Medical Abortion with Mifepristone 200 mg and Misoprostol: A Systematic Review,” Contraception 87, no. 1 (2013): 36-37; Melissa Chen and Mitchell Creinin, “Mifepristone with Buccal Misoprostol for Medical Abortion: A Systematic Review,” Obstetrics and Gynecology 126, no. 1 (2015): 12-21; Maarit Mentula et al., “Immediate Adverse Events After 2nd Trimester Termination of Pregnancy,” Human Reproduction 26, no. 4 (2011): 927-32.
[24] Catherine Vauzelle et al., “Birth Defects After Exposure to Misoprostol in the First Trimester of Pregnancy: Prospective Follow-up Study,” Reproductive Toxicology 36, (2013): 98-103.
[25] “Mifeprex (Mifepristone) Information.” FDA.
[26] Malin Helmestam et al., “Mifepristone-Exposured Human Endometrial Endothelial Cells In Vitro,” Reproductive Sciences 21, no. 3 (2014): 408-14, doi: 10.1177/1933719113497284.
[27] Ralph Miech, “Pathophysiology of Mifepristone Induced Septic Shock due to Clostridium sordellii,” The Annals of Pharmacotherapy 39, no. 9 (2005): 1483-8, doi: 10.1345/aph.1G189; Marc Fischer et al., “Fatal Toxic Shock Syndrome Associated with Clostridium Sordellii After Medical Abortion,” The New England Journal of Medicine 353, no. 22 (2005): 2352-60, doi: 10.1056/NEJMoa051620; David Aronoff et al., “ Misoprostol Impairs Female Reproductive Tract Innate Immunity Against Clostridium Sordellii,” Journal of Immunology 180, no. 12 (2008): 8222-30, doi: 10.4049/jimmunol.180.12.8222.
[28] “Mifeprex (Mifepristone) Information.” FDA.
[29] Christina Camilleri et al., “Biologic, Behavioral and Physiologic Consequences of Drug-Induced Pregnancy Termination at First-Trimester Human Equivalent in an Animal Model,” Frontiers in Neuroscience 13, no. 544 (2019): 1-21, doi: 10.3389/fnins.2019.00544.
[30] Studnicki et al., “A Longitudinal Cohort Study,” 1-8; Kathi Aultman et al., “Deaths and Severe Adverse Events After the use of Mifepristone as an Abortifacient from September 2000 to February 2019,” Issues in Law & Medicine 36, no. 1 (2021): 3-26; Margaret Gary and Donna Harrison, “Analysis of Severe Adverse Events Related to the use of Mifepristone as an Abortifacient,” The Annuals of Pharmacotherapy 40, no. 2 (2006): 191-7, doi: 10.1345/aph.1G481; Christina Cirucci, Kathi Aultman, Donna Harrison, “Mifepristone Adverse Events Identified by Planned Parenthood in 2009 and 2010 Compared to Those in the FDA Adverse Event Reporting System and Those Obtained Through the Freedom of Information Act,” Health Services Research and Managerial Epidemiology 8, (2021): 1-5, doi: 10.1177/23333928211068919.
[31] Charlotte Ellertson et al., “Accuracy of Assessment of Pregnancy Duration by Women Seeking Early Abortions,” Lancet 355 (9207): 877-81; P Taipale, V Hiilesmaa, “Predicting Delivery Date by Ultrasound and Last Menstrual Period in Early Gestation,” Obstetrics and Gynecology 97, no. 2 (2001):189-194; David Savitz et al., “Comparison of Pregnancy Dating by Last Menstrual Period, Ultrasound Scanning, and Their Combination,” American Journal of Obstetrics and Gynecology 187, no. 6 (2002): 1660-6
[32] American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins- Gynecology, “Practice Bulletin 181: Prevention of Rh D Alloimmunization,” American College of Obstetricians and Gynecologists,” August 2017, https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2017/08/prevention-of-rh-d-alloimmunization ; Christina Fiala, Michaela Fux, Kristina Gemzell-Danielsson, “Rh-Prophylaxis in Early Abortion,” Acta Obstetricia and Gynecologica Scandinavia 82, no. 10 (2003): 892-903, doi: 10.1034/j.1600-0412.2003.00266.x.
[33] Ingrid Skop, “Chemical Abortion: Risks Posed by Changes in Supervision,” Journal of the American Association of Physicians and Surgeons 27, no. 2 (2022): 56-61.
[34] Dominque Bourassa and Jocelyn Berube, “The Prevalence of Intimate Partner Violence Among Women and Teenagers Seeking Abortion Compared with Those Continuing Pregnancy. Journal of Obstetrics and Gynecology Canada 29, no. 5 (2007): 415-423, doi: 10.1016/S1701-2163(16)35493-7; “Ethical Principles for Abortion Care,” National Abortion Federation, October 2022, http://prochoice.org/wp-content/uploads/NAF_Ethical-_Principles.pdf; Megan Hall et al., “Associations Between Intimate Partner Violence and Termination of Pregnancy: a Systematic Review and Meta-Analysis,” PLOS Medicine 11, no. 1 (2014): 1-25, doi: 10.1371/journal.pmed.1001581; Laura Lederer and Christopher Wetzel, “The Health Consequences of Sex Trafficking and Their Implications for Identifying Victims in Healthcare Facilities,” Annuals of Health Law 23, (2014): 61-91, https://www.icmec.org/wp-content/uploads/2015/10/Health-Consequences-of-Sex-Trafficking-and-Implications-for-Identifying-Victims-Lederer.pdf.
[35] Hani Atrash, Finn Skjeldestad, Carol Hogue, “Ectopic Pregnancy Concurrent with Induced Abortion: Incidence and Mortality,” American Journal of Obstetrics and Gynecology 162, no. 3 (1990): 726-30, doi: 10.1016/0002-9378(90)90995-j.
[36] Laura Marion and George Meeks, “Ectopic Pregnancy: History, Incidence, Epidemiology, and Risk Factors,” Clinical Obstetrics and Gynecology 55, no. 2 (2012): 376-86, doi: 10.1097/GRF.0b013e3182516d7b.
[37] Jean Bouyer et al., “Risk Factors for Ectopic Pregnancy: A Comprehensive Analysis Based on a Large Case-Control, Population-Based Study in France,” American Journal of Epidemiology 157, no. 3 (2003): 185-94, doi: 10.1093/aje/kwf190; “FAQ155: Ectopic Pregnancy,” American College of Obstetricians and Gynecologists, February 2018, accessed May 21, 2022, https://www.acog.org/patient-resources/faqs/pregnancy/ectopic-pregnancy; American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins-Gynecology, “Practice Bulletin 193: Tubal Ectopic Pregnancy,” American College of Obstetricians and Gynecologists, Obstetrics and Gynecology 131, no. 3 (2018), doi: 10.1097/aog.0000000000002560.
[38] American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins-Gynecology, “Practice Bulletin 135: Second Trimester Abortion,” Obstetrics & Gynecology 121, no. 6 (2013):1394-1406.
[39] Klaira Lerma and Paul Blumenthal, “Current and Potential Methods for Second Trimester Abortion,” Best Practice and Research Clinical Obstetrics and Gynecology 63, (2020): 24-36, doi: 10.1016/j.bpobgyn.2019.05.006.
[40] Cates Jr. and Grimes, “Deaths from Second Trimester Abortion, 401-408.
[41] American College of Obstetricians and Gynecologists, Practice Bulletin 135, 1394-1406; Maureen Paul et al., A Clinician’s Guide to Medical and Surgical Abortion (New York: Churchill Livingston, 1999), 197-216.
[42] Stenberg v. Carhart (Thomas dissenting) 530 U.S. 2000.
[43] Mentula, et al., Immediate Adverse Events, 927-32
[44] Jennifer Kerns et al., “Disseminated Intravascular Coagulation and Hemorrhage After Dilation and Evacuation Abortion for Fetal Death,” Obstetrics and Gynecology 134, no. 4 (2019):708-713, doi: 10.1097/AOG.0000000000003460.
[45] Cates Jr. and Grimes, “Deaths from Second Trimester Abortion,” 401-408.
[46] Janet Epner, Harry Jonas, Daniel Seckinger, “Late-term Abortion,” JAMA 280, no. 8 (1998): 724-9, doi: 10.1001/jama.280.8.724.
[47] Linda Bartlett et al., “Risk Factors for Legal Induced Abortion-Related Mortality in the United States,” Obstetrics and Gynecology 103, no. 4 (2004): 729-37, doi: 10.1097/01.AOG.0000116260.81570.60.
[48] Suzanne Zane et al., “Abortion-Related Mortality in the United States: 1998-2010, Obstetrics and Gynecology 126, no. 2 (2015): 258-265, doi: 10.1097/AOG.0000000000000945.
[49] Nicole Bender et al., “The Complex Family Planning Milestone Project,” Accreditation Council for Graduate Medical Education (ACGME) and The American Board of Obstetrics and Gynecology, September 2021, accessed September 29, 2022, https://www.acgme.org/globalassets/pdfs/milestones/complexfamilyplanningmilestones2.0.pdf.
[50] W Peterson et al., “Second Trimester Abortion by Dilation and Evacuation: An Analysis of 11,747 Cases,” Obstetrics and Gynecology 62, no. 2 (1983): 185-190; Autry et al., “A Comparison of Medical Induction,” 393-397; Sarita Sonalkar et al., “Comparison of Complications Associated with Induction by Misoprostol versus Dilation and Evacuation for Second-Trimester Abortion,” International Journal of Gynecology and Obstetrics 138, no. 3 (2017): 272-275, doi: 10.1002/ijgo.12229.
[51] David Turok et al., “Second Trimester Termination of Pregnancy: A Review by Site and Procedure Type,” Contraception 77, no. 3 (2008): 155-61, doi: 10.1016/j.contraception.2007.11.004.
[52] Kerns, et al., Disseminated Intravascular Coagulation, 708-713.
[53] Jennifer Kerns et al., “A Randomized Controlled Trial of Methylergonovine Prophylaxis After Dilation and Evacuation Abortion,” Contraception 103, no. 2 (2021): 116-120, doi: 10.1016/j.contraception.2020.10.00. Kelly Fairchild et al., “Using Prophylactic Antihemorrhagic Medications in Second-Trimester Surgical Abortions,” Obstetrics and Gynecology 140, no. 4 (2022): 663-666, doi: 10.1097/AOG.0000000000004922.
[54] Mark Crutcher. Lime 5: Exploited by Choice (Denton, TX: Life Dynamics, Inc., 1996), 26.
[55] American College of Obstetricians and Gynecologists, “Practice Bulletin 135,” 1394-1406.
[56] Mentula, et al., Immediate Adverse events, 927-32; Lynn Borgatta, Nathalie Kapp, Society of Family Planning, “Clinical Guidelines. Labor Induction in the Second Trimester,” Contraception 84, no. 1 (2011): 4-18, doi: 10.1016/j.contraception.2011.02.005; Sonalkar et al., Comparison of Complications, 272-275; Kari Whitley et al., “Midtrimester Dilation and Evacuation Versus Prostaglandin Induction: A Comparison of Composite Outcomes,” American Journal of Obstetrics and Gynecology 205, no. 4 (2011): 386.e1-.e7, doi: 10.1016/j.ajog.2011.07.028.
[57] Sonalkar et al., Comparison of complications, 272-275.
[58] Stephanie Singer et al., “Fetal Survival in Second-Trimester Termination of Pregnancy Without Feticide,” Obstetrics and Gynecology 131, no. 3 (2018): 575-579, doi: 10.1097/AOG.0000000000002503.
[59] Katharine White et al., “Second-Trimester Surgical Abortion Practices in the United States,” Contraception 98, no. 2 (2018): 95-99, doi: 10.1016/j.contraception.2018.04.004.
[60] Michael Molaei et al., “Effectiveness and Safety of Digoxin to Induce Fetal Demise Prior to Second-Trimester Abortion,” Contraception 77, no. 3 (2008): 223-5, doi: 10.1016/j.contraception.2007.10.011.
[61] David Grimes, Gretchen Stuart, Elizabeth Raymond, “Feticidal Digoxin Injection Before Dilation and Evacuation Abortion: Evidence and Ethics,” Contraception 85, no. 2 (2012): 140-3, doi: 10.1016/j.contraception.2011.04.001.
[62] Stuart Derbyshire and John Bockmann, “Reconsidering Fetal Pain,” Journal of Medical Ethics 46, no. 1 (2020): 3-6, doi: 10.1136/medethics-2019-105701; “Fact Sheet: Science of Fetal Pain,” Charlotte Lozier Institute, September 13, 2022, accessed November 3, 2022, https://lozierinstitute.org/fact-sheet-science-of-fetal-pain/.
[63] Cheryl Sullenger, “Disturbing Trend: More Abortion Clinics Moving into the Late-Term Abortion Business,” Operation Rescue, January 8, 2020, accessed November 3, 2022, https://www.operationrescue.org/archives/disturbing-trend-more-abortion-clinics-moving-into-the-late-term-abortion-business/.
[64] Elizabeth Raymond and David Grimes, “The Comparative Safety of Legal Induced Abortion and Childbirth in the US,” Obstetrics and Gynecology 119, no. 2 part 1 (2012): 215-9, doi: 10.1097/AOG.0b013e31823fe923; David Reardon, “Rebuttal of Raymond and Grimes,” The Linacre Quarterly 79, no. 3 (2012): 259-260, doi: 10.1179/002436312804872730.
[65] David Reardon et al., “Deaths Associated with Pregnancy Outcome: A Record Linkage Study of Low-Income Women,” Southern Medical Journal 95, no. 8 (2002): 834-41; David Reardon and Priscilla Coleman, “Short and Long Term Mortality Rates Associated with First Pregnancy Outcome: Population Register Based Study for Denmark 1980-2004,” Medical Science Monitor 18, no. 9 (2012): 71-6, doi: 10.12659/msm.883338; Priscilla Coleman, David Reardon, Bryon Calhoun, “Reproductive History Patterns and Long-term Mortality Rates: A Danish Population-Based Record Linkage Study,” European Journal of Public Health 23, no. 4 (2013): 569-74, doi: 10.1093/eurpub/cks107; David Reardon and John Thorp, “Pregnancy Associated Death in Record Linkage Studies Relative to Delivery, Termination of Pregnancy, and Natural Losses: A Systematic Review with a Narrative Synthesis and Meta-Analysis,” SAGE Open Medicine 13, no. 5 (2017): 1-17, doi: 10.1177/2050312117740490.
[66] Mika Gissler, “Pregnancy Associated Deaths in Finland 1987-1994. Acta Obstetricia et Gynecologica Scandinavica 76, no. 7 (1997): 651-7, doi: 10.3109/00016349709024605; Mika Gissler et al., “Injury Deaths, Suicides, and Homicides Associated with Pregnancy, Finland 1987-2000,” European Journal of Public Health 15, no. 5 (2005): 459-63, doi: 10.1093/eurpub/cki042; Mika Gissler et al., “Pregnancy-Associated Mortality After Birth, Spontaneous Abortion or Induced Abortion in Finland,” American Journal Obstetrics and Gynecology 190, no. 2 (2004): 422-7, doi: 10.1016/j.ajog.2003.08.044; Mika Gissler et al., “Methods of Identifying Pregnancy Associated Deaths: Population Based Data from Finland 1987-2000,” Pediatrics and Perinatology Epidemiology 18, no. 6 (2004): 448-55, doi: 10.1111/j.1365-3016.2004.00591.x; Mika Gissler et al., “Suicides After Pregnancy in Finland, 1987-94: Register Linkage Study,” British Medical Journal 313, no. 7070 (1996): 1431-4, doi: 10.1136/bmj.313.7070.1431; Elina Karalis et al., “Decreasing Mortality During Pregnancy and for a Year After While Mortality After Termination of Pregnancy Remains High: A Population-Based Register Study of Pregnancy-Associated Deaths in Finland 2001-2012,” British Journal of Obstetrics and Gynecology 124, no. 7 (2017): 1115-1121, doi: 10.1111/1471-0528.14484.
[67] Gissler et al., Methods for identifying pregnancy-associated, 448-455; Gissler et al., Pregnancy Associated Mortality, 422-427.
[68] Additional information regarding mental health complications after abortion can be found at: David Reardon, “The Abortion and Mental Health Controversy: A Comprehensive Literature Review of Common Ground Agreements, Disagreements, Actionable Recommendations, and Research Opportunities,” SAGE Open Medicine 6, (2018): 1-38, doi:10.1177/2050312118807624.