AMA Affirms the Physician’s Role as Healer, Rejects Physician-Assisted Suicide
“Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks.”
On June 10 the American Medical Association (AMA) voted 360-190 to affirm Report 2 of The Council on Ethical and Judicial Affairs (CEJA 2), a nuanced report that ultimately favors maintaining AMA opposition to physician-assisted suicide. Further, a second vote by the House of Delegates yielded 71% of votes reaffirming opposition to physician-assisted suicide.
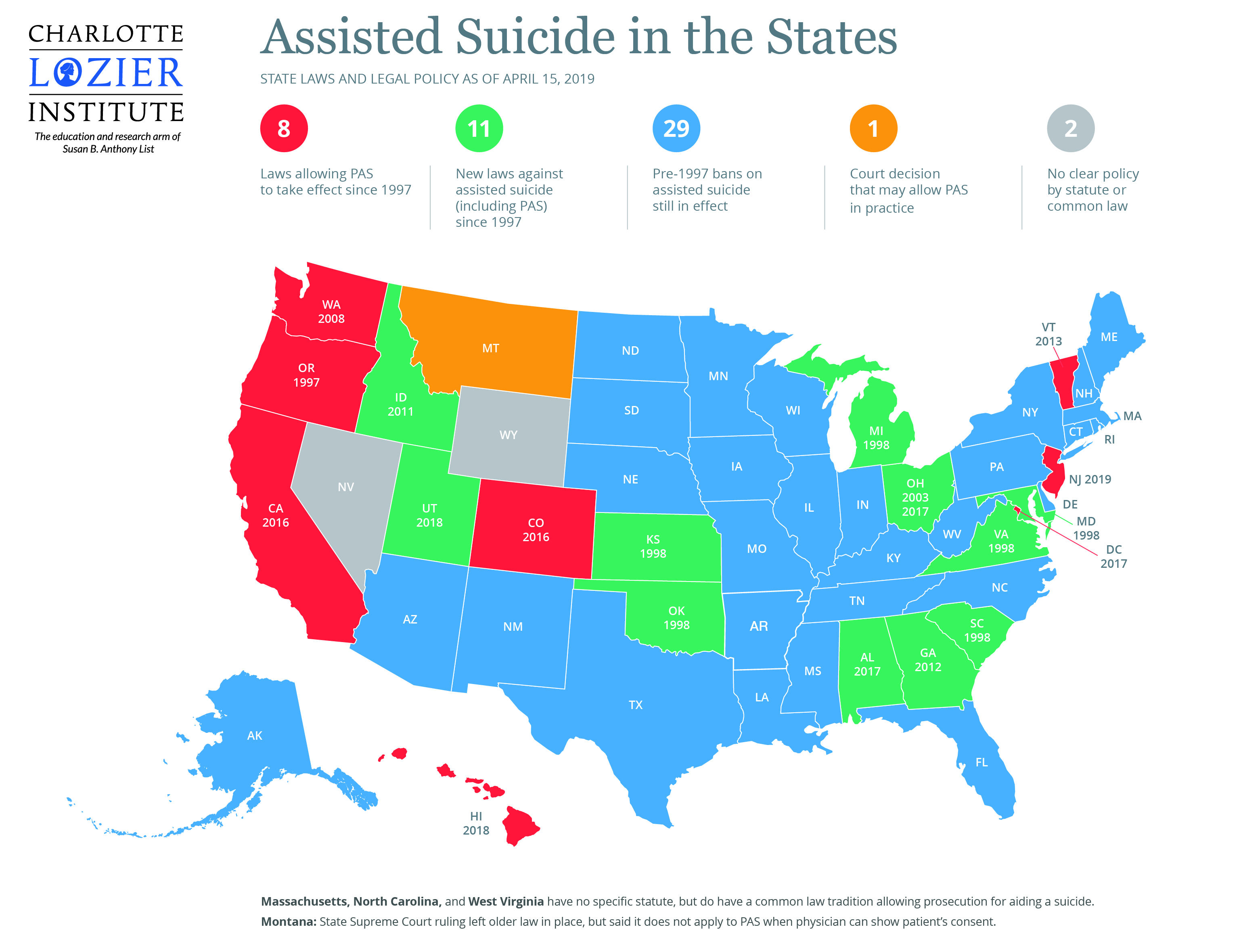
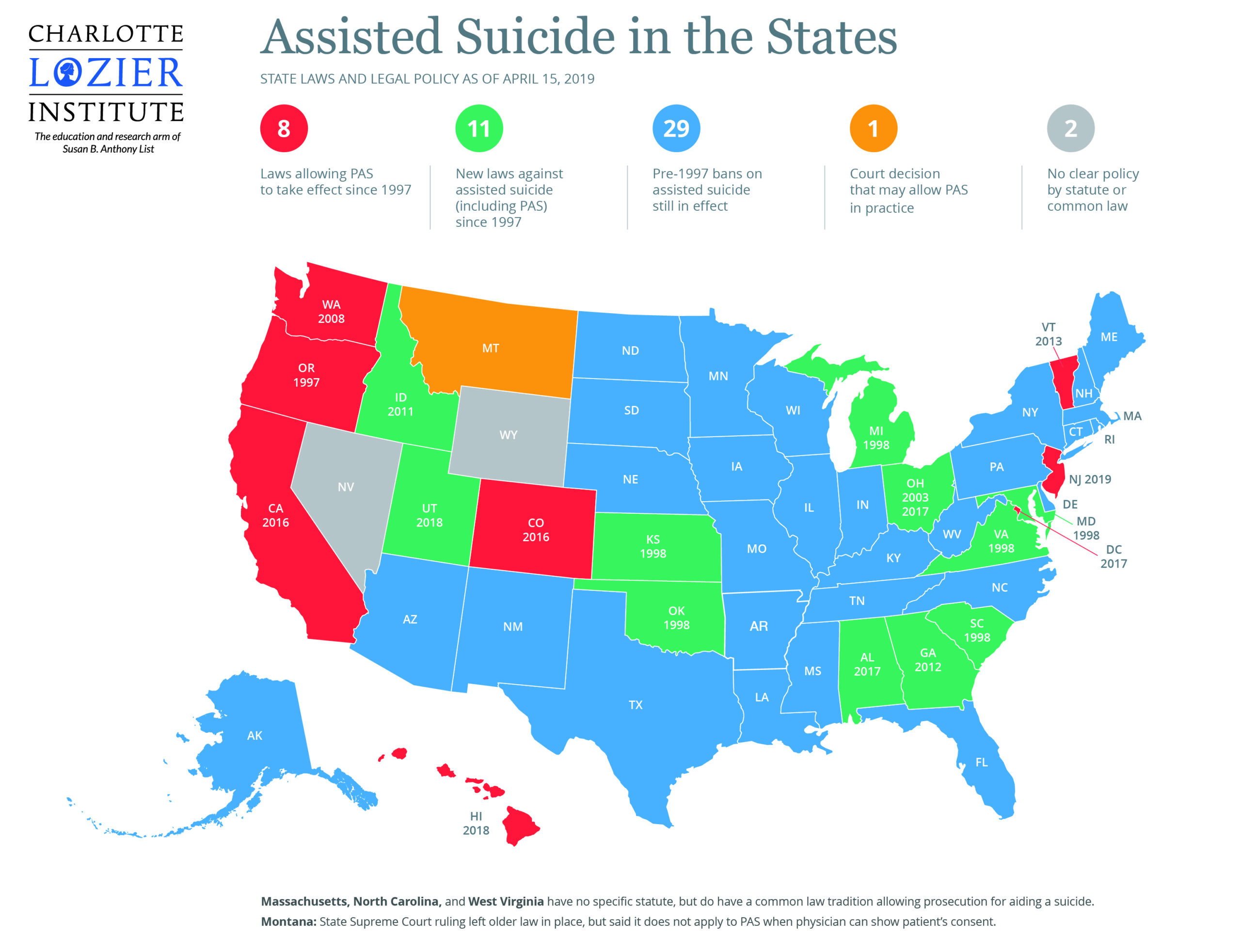
CEJA, the AMA’s Council on Ethical & Judicial Affairs which determines the AMA’s Code of ethics, has considered the subject of physician-assisted suicide twice in 2018 alone and has recommended each time that the AMA maintain its opposition to the practice. CEJA’s studies responded to the AMA House of Delegate’s request to “study the issue of aid in dying with consideration of data collected from the states that currently authorize aid-in-dying, and input from some of the physicians who have provided medical aid-in-dying to qualified patients…[and] to distinguish between ‘physician-assisted suicide’ and ‘aid in dying.’” Regarding the latter, the council decided that “despite its negative connotations, the term ‘physician assisted suicide’ describes the practice with the greatest precision.”
The CEJA 2 report is valuable for other reasons in addition to its role in preserving the AMA’s historical stance on assisted suicide. Perhaps one of the most important of these is the recognition by both advocates and opponents of physician-assisted suicide of the need to make end-of-life care accessible to patients across a spectrum of backgrounds. CEJA 2 documented this recognition that occurred at an open forum:
“[P]atients and physicians too often still do not have the conversations they should about death and dying, and…too few patients are aware of the range of options for end-of-life care, raising concern that many patients may be led to request assisted suicide because they don’t understand the degree of relief of suffering state-of-the-art palliative care can offer. Participants who in other respects held very different views concurred as well that patients may be vulnerable to coercion, particularly patients who are in other ways disadvantaged; and expressed concern in common that forces external to medicine could adversely influence practice.”
Further, CEJA 2 brings to light a poignant observation made at a workshop on physician-assisted death sponsored by the National Academies of Science, Engineering and Medicine: “…[I]t is [important] to understand why a patient requests assisted suicide as a starting point for care.” This is a monumental and extremely insightful statement. End-of-life care is unique in that death does not have a cure. There is no vaccine against death, nor a magic potion to dispel its inevitability. Death is the end of life, which can be accepted in peace, or brought about in anguish with a desperation and deep desire to reach a place of peace. A person seeking physician-assisted suicide is deeply seeking peace. This is essential for medical professionals to understand. Death is not sought for its own sake, it is sought to relieve suffering. The relief of suffering and the acceptance of death – not the remedy of death or the attempt to use death as a “treatment” to relieve suffering – is the foundation of an end-of-life care compatible with the innate dignity of the human person.
CEJA 2 opens further discussion about the need to understand why individuals might choose physician-assisted suicide, and how to respond. Requests for physician-assisted suicide show the deep suffering that patients can experience, whether physical, spiritual, or psychological, and the need to address those issues before they escalate to the point of a patient requesting physician-assisted suicide. While such requests are saddening, CEJA 2 points out that physicians have the opportunity to “respond creatively to the patient’s needs other than providing the means to end life—by such means as better managing symptoms, arranging for psychosocial or spiritual support, treating depression, and helping the patient to understand more clearly how the future is likely to unfold.” Farr Curlin, a physician and professor at Duke University, stated, “I can tell you that we now have measures to effectively treat pain, breathlessness, and other difficult symptoms more than we have ever had before… And we can do that while respecting ethical guidelines that have guided the profession of medicine for centuries.” Medical professionals and policy makers must be at the forefront of understanding the reality of life and death, the ethics of end-of-life care, and the place of modern technology in the ageless event of death.
On June 10, therefore, the AMA made a decision to uphold not only the dignity of the dying, but the integrity of the entire medical profession. The decision of the AMA, however, is not the only important decision to be made. Keeping the evil of physician-assisted suicide at bay is an effort that takes the attention of the entire community. Charlotte Lozier Institute associate scholar Bobby Schindler says, “Naturally, no one wants to find themselves in a situation of diminished autonomy or independence, let alone disability or injury. But in our daily lives, we can do better by choosing to love, care, comfort, and encourage individuals facing these trying situations.” He continues:
“What this means, practically speaking, is developing a willingness to heroically witness a culture of life and love in our own lives, in our own families, and in our own neighborhoods. Just as important as public advocacy, legislative efforts, and so forth, are concrete actions like taking an ailing family member into our homes, helping care for them, looking after them, and visiting and loving those forgotten in hospice, nursing homes, and other facilities.”
Physicians and individuals must show courage and willingness to uphold the true dignity of human life, not only at its origin, but at its end.
Hannah Howard, M.S. is a research associate at the Charlotte Lozier Institute